CUE INFOMERCIAL: I’m here today to tell you about a miraculous substance that will significantly increase your cognitive function, clear your head and improve your night vision. It is absolutely legal with proven safety and reliability, and you will see immediate improvement in your physical, mental and visual performance. You are probably asking, what is this miracle substance? The answer is supplemental oxygen, and you can buy it at an FBO near you.
Shortly after I splurged on my first aircraft, my dad excitedly offered to buy me an aviation accessory. Was there anything I could use to improve my safety, but likely wouldn’t buy for myself? I looked at my shopping list and suggested supplemental oxygen equipment. At the time, it seemed like a luxury I could delay, but it turned out to be one of the most valuable aviation accessories I own. It demonstrated its value right away. With it, I had the ability to leisurely cruise-climb up and over mountain passes. On cross-country flights, I climbed to where I could pick up 30-to-60-knot tailwinds. In winter, when intermittent cloud tops are often around 11-14,000 feet, I could avoid them by getting on top. As a simple GA pilot, supplemental oxygen was a game changer.
More than a decade later, I find myself increasingly reaching for oxygen at lower and lower altitudes, particularly at night. This miracle inhalant has dual properties: it not only increases cognitive ability, but also improves night vision.
“I don’t have any specific data, but anecdotally, it seems like an increasing number of pilots are flying with supplemental oxygen systems,” said Dr. Brent Blue. Blue is an FAA Senior Aviation Medical Examiner and a frequent lecturer in the areas of aviation medicine, hypoxia and carbon monoxide poisoning. In 1994, he and partner Mike Busch founded Aeromedix.com to help bring oxygen aids, like pulse oximeters, and other equipment into regular use in general aviation.

For its size, the brain is an oxygen-demanding organ. In adults, the brain accounts for only 2-3 percent of total body weight, but brain activity accounts for 20-30 percent of energy consumption, and consumes approximately 200 liters of oxygen per day just for baseline metabolic functioning.
Brain cells are very sensitive to a lack of oxygen, brain hypoxia, which can rapidly cause severe brain damage or death. An unconscious person who is not breathing can suffer permanent brain damage after only four minutes without oxygen.
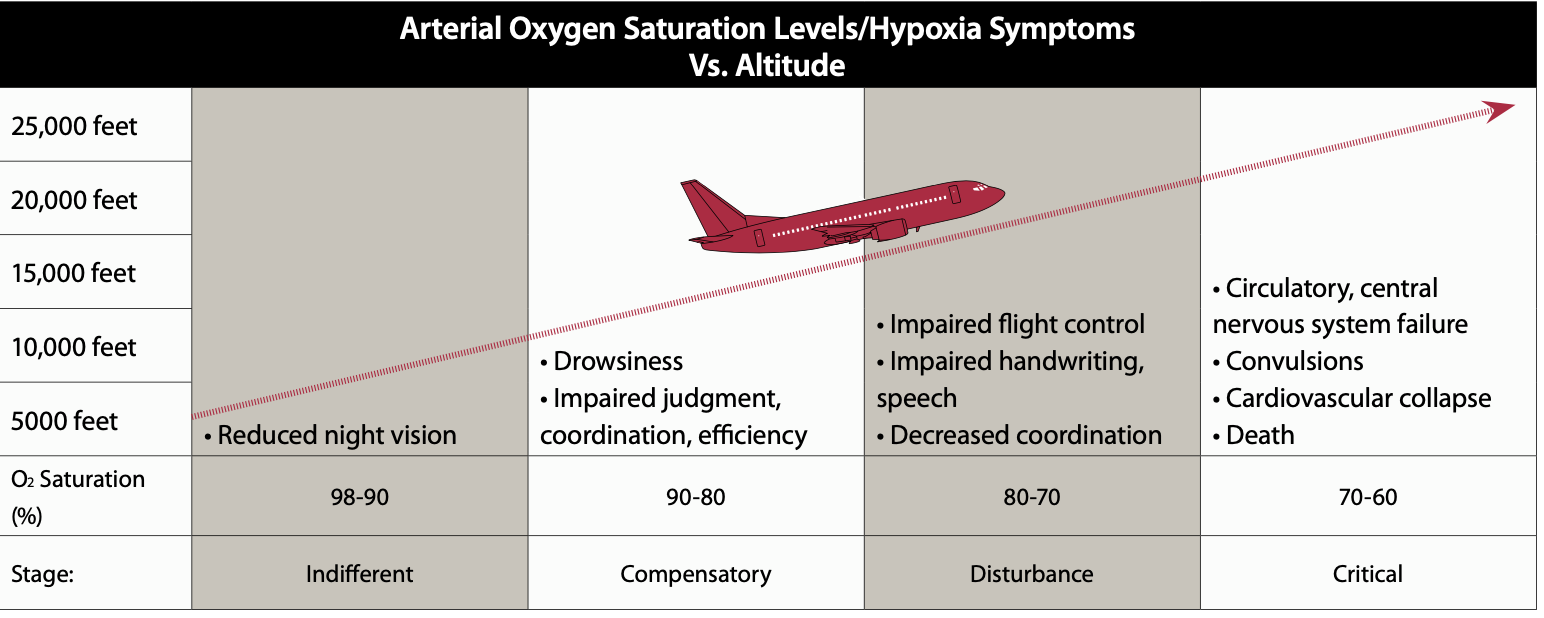
Hypoxia from lack of oxygen at altitude is usually not so severe that it causes permanent brain damage, but numerous studies demonstrate that acute hypoxia results in lower cognitive function. Flying while hypoxic is equivalent to flying impaired. Put more simply, it is flying while stupid.
The good news is that people with fully saturated blood oxygen above their typical baseline perform demonstrably better on cognitive tests. For pilots, that means if you can get your oxygen levels higher than your baseline, you will more likely have a performance edge.
SAFE VS. LEGAL
According to Blue, FAA rules on supplemental oxygen were mostly designed to promote rather than inhibit aviation. They provide just enough latitude for us to navigate up and over high passes in the Western U.S. without pressurization or the burden of oxygen systems that were prohibitively expensive at the time. So if you thought the FAA’s altitude-based oxygen rules are designed primarily around medical and physiological data, you would be wrong.
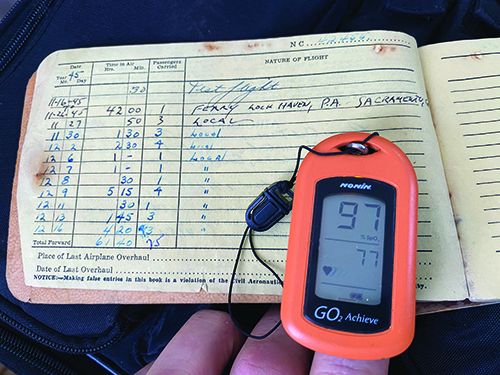
Blue has a simple 5-10 rule of thumb for knowing your own particular oxygen needs, as individual to you as your weight or height: “Start at your home base by using a pulse oximeter to measure your baseline blood oxygen saturation level. At flying altitude, when your blood oxygen level has dropped by five percentage points off your baseline, you should be on oxygen. If or when your oxygen saturation drops below 10 percent off your baseline, you need to be on oxygen.” This rule of thumb factors in your individual baseline physiology and the altitude of your home.

The sales pitch concluding this infomercial is: If you are flying a lot of cross-country flights at altitude or a lot of night flights, you should seriously consider purchasing a supplemental oxygen kit and a pulse oximeter. Accessing higher altitudes will decrease your fuel burn, since thinner air means leaner mixtures, and might open up more efficient route possibilities that involve higher mountain passes.
Supplemental oxygen sharpens the weakest link in general aviation, the loose nut between the rudders and the yoke. It improves pilot safety by reducing potential cognitive losses due to hypoxia, and if it raises your baseline blood oxygen levels, may actually improve cognitive function.
Bottom line, if you are considering a night flight at any altitude, oxygen is a known performance-enhancing inhalant. With such attributes, it seems like a no-brainer. If you haven’t acquired your system yet, you may want to check your blood oxygen levels because you may not be thinking clearly.
Doc Blue’s 5-10 rule is useful because pilot physiology and acclimatization are baked in. Pilots living at higher altitudes where there is less oxygen typically have lower blood oxygen levels in their blood, but they are acclimated to deal with it by having more red blood cells. Think of the energy delivered to your body as a 100-car coal train, each car 100-percent full at sea level. At altitude, that same train of energy may only be 90-percent full. The only way to supply the missing energy is to add more cars. In this metaphor, red blood cells are the extra cars. Someone who lives in Denver or Sante Fe, both at higher altitudes, may still have a full load with a baseline 92-percent blood-oxygen saturation because they have more blood cells carrying the freight. It depends on your home base.
“From medical studies of mountaineers, we know that our bodies adapt to living at altitude,” said Blue. “It takes the human body roughly 90 days at a given altitude to acclimatize through the production of extra red blood cells to carry the lower pressure oxygen. You can’t go by an absolute number, say, 92-percent blood oxygen for example, as the threshold for needing supplemental oxygen because a person living at altitude may have 92 percent as their baseline and not need supplemental oxygen. Meanwhile, a person coming from sea level, whose oxygen levels are typically around 100 percent, may desperately need oxygen when they have dropped to 92 percent.”
Regardless of what altitude you are flying, Blue’s 5-10 rule will keep you safe and the FAA’s regulatory altitude (where oxygen is required) will keep you legal. For any given person, the two may or may not always correspond.
OXYGEN AND LONGEVITY
In addition to acclimatization and red blood cell count, there are three other factors affecting blood oxygen levels. “The four greatest factors affecting longevity are: 1) heredity, 2) smoking and exposure to tobacco products, 3) body weight and 4) exercise,” said Blue. “You don’t get to pick your parents so you have no control over the first one. But the remaining three factors, which are known to extend life, also affect oxygen uptake at altitude.”
The first controllable factor is smoking and tobacco. Blue says if you smoke, vape or consume other smoky inhalants, you are damaging your respiratory system and making it less able to do its job. “The damage from smoking or vaping not only reduces your body’s ability to deliver oxygen to the blood, it increases your susceptibility to respiratory infections such as bronchitis, the flu or COVID-19,” said Blue. “Don’t smoke.”
Next is obesity. “There is no delicate way to put it,” said Blue, “but if you are obese, you are going to have significantly more oxygen issues than someone who is at their ideal weight.” This isn’t fat-shaming; it is just the relationship between physiognomy and the act of breathing, particularly when sitting. “The compression of the pulmonary cavity, when it is physically displaced by body fat, makes it harder and harder to draw a deep enough breath,” said Blue. “The more fat in the pulmonary cavity, the less room for lung expansion.”
The third controllable factor, weight, is actually addressed by the FAA from a regulatory perspective. This is because some obese pilots will suffer from sleep apnea, which interrupts sleep cycles and results in inadequate rest. Blue believes that because obesity interferes with the ability to draw deep-enough breaths while seated, it is also an aeromedical factor that is clearly detrimental to a pilot’s ability to intake sufficient oxygen.
Exercise is the fourth factor that Blue cites as affecting oxygen uptake. He recommends at least 30 minutes of exercise every day, with a sustained heart rate in the medical target zone of 70-85 percent of your maximum heart rate. Maximum heart rate is equivalent to subtracting your age in years from 220. I calculated it for my 56-year-old self: 220-56=164, so I need to exercise at least 30 minutes every day with a heart rate consistently between 115-139 (70-85 percent). And seven days a week.
“Really?” I asked, cringing. Blue says, “If you seriously strive for seven days a week, you should be able to actually manage 4-5 days a week. If you aim for 4-5 days, chances are you will only hit a couple days. Compliance goes down. It isn’t easy, but if you want to live long and fly at altitude, I recommend 30 minutes of real sustained heart rate exercise, and yes, seven days a week. The key is working it into your schedule and finding activities that you can, at a minimum, tolerate, but better yet, enjoy.”
There is no practical difference between aviator’s breathing oxygen and oxygen used for medicine or welding. This wasn’t always the case.
In the 1950s and 1960s, medical oxygen was humidified, which could result in frozen lines at altitude. Today, humidification of medical oxygen happens in the healthcare facility after it leaves the tank.
Although legally a built-in aviation oxygen system must be filled by an A&P with expensive aviator’s oxygen (which is tested for water), portable systems can be filled at your local oxygen supplier for a fraction of the cost. Some suppliers will require a prescription, which Dr. Blue will be happy to send to anyone who wants one for free. Just email him: [email protected].
FINALLY, NIGHT VISION
If you’re still not convinced of supplemental oxygen’s value to pilots, consider night operations. Night vision is dominated by rod cells, which are on the periphery of the retina. The less light-sensitive cones, which provide color vision, are concentrated in the center of the visual field. A result is that we tend to have slight tunnel blindness at night, because the least-sensitive receptors are in the main focal field, while our peripheral vision is more sensitive.
Just as the brain is an energy/oxygen hog, the same is true for the rods and cones. A 2006 paper, published in the journal “Vision Research,” looked at the effects of hypoxia (low oxygen), hypocapnia (low carbon dioxide) and hyperoxia (high oxygen) on night vision, compared to normal oxygen levels. The conclusion was that “…aircrew should consider using supplementary oxygen if they are reliant upon viewing scotopic external scenes (less than full moonlight) when flying at night.” It went on to conclude, “At night, supplementary oxygen may benefit aircrew visual sensitivity, even at ground level.”
If you spend much time in unpressurized aircraft at or above 10,000 feet, or at night above 5000 feet, supplemental oxygen—and a pulse oximeter—should be considered mandatory equipment.

Pulse oximeters have another, possibly equally helpful self-diagnostic use as recounted in a recent New York Times opinion piece by Dr. Richard Levitan. Levitan wrote about his recent experience as an ER doctor at New York’s Bellevue hospital and identified pulse oximeters as a valuable, potential life-saving tool for early detection of more serious Covid-19 pneumonia.
He noted that the signaling to our brain that we need to take a breath isn’t driven by low blood oxygen levels, but rather the buildup of carbon dioxide. In typical pneumonia cases, patients suffer from both low oxygen and carbon-dioxide buildup. The result is uncomfortable gasping for air and shortness of breath, an early warning that something is deeply wrong with the respiratory system.
“Pulse oximeters helped save the lives of two emergency physicians I know, alerting them early on to the need for treatment,” Levitan wrote in the Times. “When they noticed their oxygen levels declining, both went to the hospital and recovered (though one waited longer and required more treatment).”




Excellent article!
Would you be so kind as to please pass this note on to Dr. Blue?
Sent June 9
Dr. Brent Blue
President & Founder
Oxygen To Go
555 Deer Drive, Unit 205
PO Box 8880
Jackson, WY 83001
Dear Mr. Blue, We rented one of your portable oxygen concentrator units to travel with us from Colorado to Puerto Vallarta, Mexico on behalf of our 83-year-old Mom, Vicki Porter. We’re writing to let you know that although your front-of-house customer service expedited our order with skill and kindness, your on-call Technician was insulting, unprofessional, unhelpful, and as a representative for the life-saving device showed a blatant disregard for life.
On the evening of June 5th, while staying at a five-star resort, your machine sounded a warning, the wrench light appeared, and then the machine shut down. My sister used her cell phone to make the international call to your customer service line as advised. Mr. David Hughes took our call and advised us that the machine would need to be reset. We asked him to please walk us through the re-set steps. He told us the battery would need to come off the back of the unit. We informed him that there was no battery on the back of the unit and that the unit was being powered by electricity. The news that we were traveling without a battery and in Mexico triggered Mr. Hughes. His brief attempt to guide us out of the emergency situation quickly became an angry monologue about how he would never travel to a third-world country and that Mexicans don’t even want to be in Mexico and then finally, at the close of his nasty rant, he added that the Mexican electricity fried your unit. Mr. Hughes continued to talk over my sister, who was still trying to find a solution to our problem.
What can we do, she asked.
You can go to your concierge and tell him! Mr. Hughes barked.
Tell the concierge what, she asked slowly?
Tell him that you need oxygen.
That was the final instruction from your frustrating and ineffectual on-call technician. Shame on him.
We dialed your 1-800 number again promptly, made a report about the belligerent Mr. Hughes, asked if we could speak with another technician and were told that he was the only help available. Imagine our shock and disappointment when we discovered that Mr. Hughes was the only tech on call and even bigger shock and disappointment when we discovered that he is your Director of Operations for Oxygen To Go.
Mr. Hughes also thoughtlessly referred to Vicki as the patient instead of a client, which made her feel belittled. And his inept handling of our need for technical support left your client, our mother, Vicki, with sleepless anxiety.
Mr. Hughes’ unnecessary tone and personal comments about Mexico left Vicki’s daughters (me and my sister) dumbfounded at not only how poorly we’d just been handled by Oxygen To Go, but more importantly without a solution to our problem!
In closing, David Huges’s idea of customer service was not a service at all. He was insulting, unprofessional, and, as a representative for the device showed a blatant disregard for human life. Vicki’s rental bill as well as the cost for t twenty-two-minute international call should be 100% covered by your company as a show of good faith.
We look forward to hearing from you.
Sincerely, Client – not patient – Vicki Porter
Daughter, Tracy Porter
Daughter, Terri Porter
23744 Hilltop Road
Buffalo Creek, Colorado 80425
303.838.4164